Diabetes & Diabetic Retinopathy
Diabetes is a systemic condition characterized by high blood sugar due to the lack of insulin. Type I has an autoimmune source whereas type II is due to the pancreas not producing enough insulin.
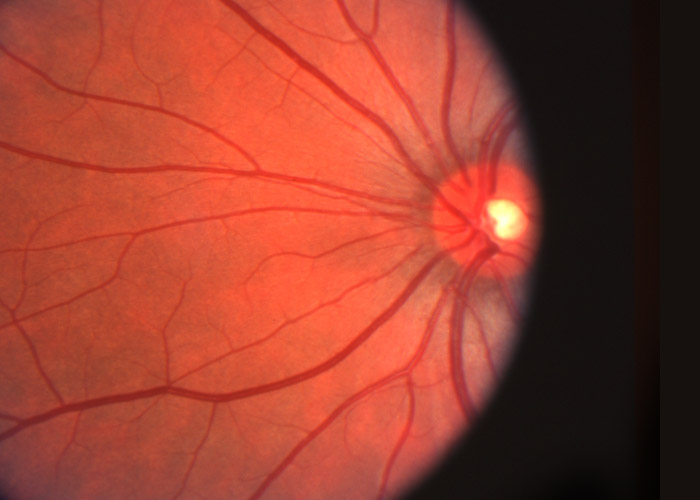
Poorly controlled diabetes can affect the eyes. Diabetes is the leading cause of blindness in Canada. Vision loss is due to changes that occur at the back of the eye, the retina. This dictates regular eye examinations, in particular dilated examinations, in order to monitor the health of the eyes. These retinal changes, termed diabetic retinopathy, are not necessarily present in all diabetic patients. Diabetic retinopathy can be divided into nonproliferative and proliferative.
Nonproliferative diabetic retinopathy (NPDR) includes three stages: mild, moderate and severe. Mild NPDR consists of microaneurysms only (outpouchings of capillary walls in the retina). Moderate NPDR ranges between mild and severe NPDR. It exhibits signs of blood vessel blockages, such as cotton wool spots, hard exudates, dot and blot hemorrhages and venous beading. Severe NPDR can involve any one of the following presentations: four quadrants of hemorrhages, two quadrants of venous beading, and one quadrant of IRMA (intraretinal microvascular abnormalities). IRMA, also known as shunt vessels, is considered a precursor to proliferative disease. Proliferative diabetic retinopathy (PDR) encompasses neovascularization, the growth of new leaky blood vessels, as well as preretinal and vitreous hemorrhages. These hemorrhages have serious affects on vision resulting in emergency visits, with symptoms ranging from blurry and fluctuating vision, dark areas of vision, floaters, difficulty distinguishing colors and vision loss.
Macular edema is the swelling of the retinal area that is responsible for central vision and detail. It can occur at any stage of retinopathy and is another culprit of serious vision loss. If it fulfills certain criteria it becomes clinically significant, making treatment necessary. Symptoms include vision loss, especially difficulty in seeing colors and details.
Both PDR and clinically significant macular edema require treatment. PDR is treated with a laser technique called panretinal photocoagulation. This involves killing off the blood supply to the peripheral retina, so that blood is directed to the macula. Similar treatment for macular edema is also used, in the form of a focal or grid laser. Along with laser, anti-VEGF or corticosteroid injections are often used in management. VEGF is a growth factor that promotes neovascularization, thus anti-VEGF injections are an attempt of preventing further neovascularization. Corticosteroid injections are used to treat the swelling and inflammation occurring in the retina. In some cases a vitrectomy may be indicated. It involves the removal of the vitreous, a gel like substance, from the eye. It is indicated when there is a lot of hemorrhaging, a retinal detachment has occurred, or if extensive neovascularization is present.
Diabetic patients must be monitored carefully and have their eyes checked regularly. Progression determines the frequency of visits to the optometrist. If no ocular signs are present, an annual dilated fundus exam is the standard of care. This is increased to every 6-9 months once mild NPDR is suspected, and every 4-6 months if moderate or severe NPDR is established. PDR requires eye examinations at every 2-3 months.
For more information, please call us or visit our Beyond Vision optometry at Millwoods, Edmonton today.

